- mouth
- skin
- intestines
- respiratory system
- urinary tract
When this condition is caused by bacteria, it’s also known as bacterial endocarditis. In rare cases, it can also be caused by fungi or other microorganisms.
DEFINITION :
Infective or bacterial endoarditis {IE OR BE} is serious infection of the valvular and mural(wall) endocardium caused by different forms of microorganism and is characterised by typical infected and friable (easily brakable) vegitation.
Vegetation.: which is a mass of platelets, fibrin, microcolonies of microorganisms, and scant inflammatory cells.
ETIOLOGY :
Endocarditis occurs when germs enter your bloodstream, travel to your heart, and attach to abnormal heart valves or damaged heart tissue. Certain types of bacteria cause most cases, but fungi or other microorganisms also may be responsible.
1. Staphylococcus aureus (45-65%) :
- most common cause of acute Infective endocarditis
- high virulence
- found in skin ,enter through IV drug usage
- it attacks healthy valves
- it forms large vegetation (multiplication of bacteria)
- most common cause of subacute infective endocarditis
- low virulence
- found in mouth,enter through dental procedures
- it attacks previously damaged valves
- it forms small vegetation
3.Staphylocaccus epidermidis :
- it transmitted via infected peripheral venous catheter and during valve surgery
- it affects Prosthetic valve or pace maker/implantable cardioverter defibrillator
4.Enterococcus faecalis , Streptococcus bovis (10%)
- found in gut
- during colorectal cancer or ulcerative colitis it enters into blood stream
H- Haemophillus species
A- Aggregatibacter
C- Corynebacterium
E- Eikenella
K- Kingella
- gram negative group
- normal flora of mouth and throat
- enter into blood in patient with poor dental hygine or periodental infection
- transmitted from infected animal
- starting Q fever after several months develope into endocarditis
Risk factors :
1.Sex - male
2.Age - >60 years
3.Pre - existing conditions
- Previous infective endocarditis
- Pre damaged or prosthetic heart valves
- Congenital heart defects
- Chronic haemodylasis
- Immunosupressive
4.Bacteremia (condition leads to cause bacteria in blood)
- infected peripheral venous catheter,surgery,dental procedures
- IV drug abuse (non sterile venous injection)
- bacterial infection of various organs Eg : Urinary tract infection (UTI),Spondlodiscitis
- It is a fulminant (sudden onset) and destructive acute infection of the endocardium by highly virulent bacteria in a previously normal heart
- It runs around 2-6 weeks
- lenta -slow
- It is caused by less virulent bacteria in previously diseased heart
- Its course runs from 6weeks to few months sometimes years
- fever and chills -90% of case
- tachycardia (increased heart rate)
- dyspnea,cough,pleuritic chest pain
- Arthralgias (joint pain)
- Myalgia (muscle pain)
- Mitral valve regurgitation -holosystolic murmur
- Tricuspid valve regurgitation -holosystolic murmur
- Aortic valve regurgitstion -early diastolic
-Signs of progressive heart failure (edema,dyspnea)
- PETECHIAE :splinter hemorrhage (septic emboli in nails)
- JANEWAY LESIONS :small,nontender,erythematous macules on palm and soles
- Splenomegaly and left upper quadrent of abdominal pain
- NEUROLOGICAL - eg: seizure,paresis,due to septic embolic stroke
- signs of pulmonary emboli eg: dyspnea
- arthritis
- multiple blood culture -to find out the organism involved
- the blood culture may shows LEUKOCYTOSIS (increase in white blood cells)
2.Echocardiography:
- Detects valve vegetation
- Transthoracic echocardiography (TTE) – 75% sensitive
- Transesophageal echocardiography (TEE) -90% sensitive
3.Modified Duke criteria :
To confirm the diagnosis
one of the following requirements must be met
- Two major criteria
- One major and three minor criteria
- Five minor criteria
Major diagnostic
criteria :
- Two separate blood culture positive for typical pathogen
- Evidence of endocardial involvement in echocardiogram
Minor diagnostic
criteria :
- Predisposition: underlying heart diseases or IV drug
- Fever ≥38º C [100.4F]
- Vascular abnormalities – Arterial emboli,septic infract
- Immunologic disorders – Glomerulonephritis,osler node
- Microbiology – positive blood culture
DIFFERENTIAL DIAGNOSIS :
1. Non infective endocarditis :
refers to formation of sterile platelet and fibrin thrombi on cardiac valves and adjacent endocardium in response to trauma, circulating immune complexes, vasculitis, or a hypercoagulable state.
2. Prosthetic valve thrombosis :
TREATMENT :
Empirical theraphy:
It is the antibiotic theraphy started as soon as the patient arrives to hospital on the experience of pysician (a guess) without knowing the exact microorganism.after the results came from lab the antibiotic regimens change according to the organsim.
1.Native valve :
Initial IV empric
antibiotic treatment with vancomycin then adopt IV antibiotic to blood culture
- 4week treatment
Drug of choice :
Penicilline G
- 2week treatment
Drug of choice :
Gentamicin+ Penicilline G
2.Prosthetic valves:
Same antibiotics as
native valve but longer duration the antibiotics are given atleast 6weeks
3.IV DRUG users :
- IV Vancomycin
After confirmation of susceptible
pathogen
- IV nafcillin – 2weeks
- Po cloxillin - (2weeks)
4.HACEK organism :
Drug ofchoice : First
line – 3rd and 4th generation IV Cephalosporin
Second
line – Ampicillin-sulbactam,IV fluroquinolone
Duration : Native valve
– 4weeks
Prosthetic valve – 6weeks
5.Surgery :
Surgery for Infective Endocarditis (IE)
Surgical treatment of infective endocarditis is aimed at:
- Removal of all infected tissue
- Drainage of abscesses (collection of pus)
- Repair of the heart tissue
- Repair or replacement of the affected valve
Surgery for endocarditis is very specialized and demanding. It requires extensive experience and familiarity with different reconstructive methods including the use of homografts (human cadaver valves). Transesophageal echocardiograms (TEE) performed before, during and after surgery help to guide the surgeon and ensure valve function is optimal.
Debridement - removal of infected tissue. If the infection has affected only the valve leaflets (cusps), removal of the infected matter will be sufficient. However, if the infection has affected more of the valve or into the heart tissue, then debridement will require a more technically difficult approach.
Valve reconstruction - depending on the specific surgical case, the surgeon will repair the valve or replace the valve with a new valve (valve prosthesis). The prosthesis may be biological, mechanical or a homograft. The homograft has proven to be particularly effective in cases with severe aortic valve endocarditis. In some cases of aortic valve IE, the Ross Procedure may be used
.
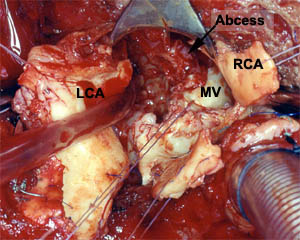
Aortic Valve: destructive endocarditis caused by staph aureus, with abscess cavity under the pulmonary artery (aortic valve removed) (RCA - right coronary artery, LCA - left coronary artery, MV - mitral valve)
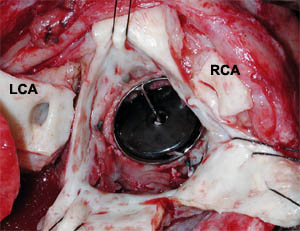
Aortic Valve: Prosthetic valve endocarditis with circumferential infection and dehiscence of the valve posteriorly (RCA - right coronary artery, LCA - left coronary artery)
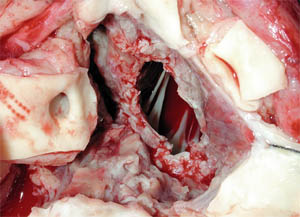
Aortic valve: same valve after debridement, cleaning up
Aortic Valve Endocarditis: After debridement (cleaning) and reconstruction with a homograft.
COMPLICATION :
, endocarditis can cause several major complications, including:
- Heart problems, such as heart murmur, heart valve damage and heart failure
- Stroke
- Seizure
- Loss of the ability to move part of all of your body (paralysis)
- Pockets of collected pus (abscesses) that develop in the heart, brain, lungs and other organs
- Pulmonary embolism — an infected vegetation that travels to the lungs and blocks a lung artery
- Kidney damage
- Enlarged spleen























0 Comments